Migraines cause prolonged episodes of intense suffering, with debilitating pain that has significant professional and social repercussions. Find out what can cause migraines and how they can be treated.
What is a migraine?
A migraine is a primary headache characterised by recurring episodes of severe throbbing or pulsing pain. In addition to a debilitating headache, it can be accompanied by nausea, vomiting and heightened sensitivity to sound, light or odours.
Migraines can occur at any age, but are more common in young adults. In many cases, they tend to become less intense or disappear after the age of 50. This neurological disorder affects approximately 14% of the global population and is almost twice as prevalent in women than in men - this difference is believed to be influenced by female oestrogens.
What are the types of migraines and their symptoms?
Migraines are considered the third most predominant disorder in the world. They can be divided into three primary categories: migraine with aura, migraine without aura and chronic migraine.
Migraine with aura
A migraine with aura is characterised by a set of sensory and perceptual distortions. The most common signs include seeing black or bright spots, tingling sensations or the inability to speak clearly. These signs are temporary and completely reversible, and usually occur before pain.
Silent migraine
Migraines can also occur without pain, and these silent migraines only present signs such as temporary visual disturbances or nausea.
Ocular migraine
This type of migraine causes temporary vision loss in one eye and is more common in women during their fertile years. In this case, it’s important to seek immediate medical attention, as it can lead to more serious complications.
Vestibular migraine
Patients with vestibular migraine experience symptoms associated with vertigo, in other words, imbalance and motion sensitivity, causing unsteadiness. Dizziness can also occur.
Chronic migraine
Migraines are considered chronic when patients are afflicted with this neurological disorder for at least 15 days per month, reaching high levels of disability.
What is the average duration of a migraine?
Migraine attacks can last for hours or days, with symptoms worsening over the first few hours. Typically, episodes follow the phases below:
Prodrome
In this phase, there are signals of an impending attack. Warning signs can include fatigue, difficulty concentrating, changes in appetite and/or mood swings, irritability or agitation.
Aura
At this stage, symptoms are more severe and may include a series of visual and perceptual distortions. These alterations are a normal migraine symptom and do not indicate neurological or visual damage. Not all patients experience this phase.
Headache
During this phase, pain is intense and aggravated by movement. Typically, migraines diminish during sleep. They can also cause nausea, vomiting and extreme sensitivity to light and/or sound. Severe attacks can disrupt family and professional life.
Postdrome
This is the final phase, characterised by a gradual decrease in symptoms. In some cases, the attack can also disappear suddenly. Many patients report feeling “hungover” after an attack.
Migraine: causes
Migraines are caused by the dilation of cerebral blood vessels which can have several causes that are still relatively unknown. However, certain factors have been identified which, although they do not cause migraines, may trigger or aggravate attacks. These factors can vary from person to person.
The most common are:
- Insomnia;
- Climate changes;
- Fasting or skipping meals;
- Excessive sensory stimulation;
- Stress;
- High oestrogen levels.
Although the cause-and-effect is still unclear, certain foods, such as aged cheeses, chocolate, alcohol, shellfish, strawberries, processed foods or excessive caffeine, have been associated with migraines. Furthermore, there may be a genetic predisposition, meaning that patients with a family history of migraine are more likely to develop this neurological disorder.
How are migraines diagnosed?
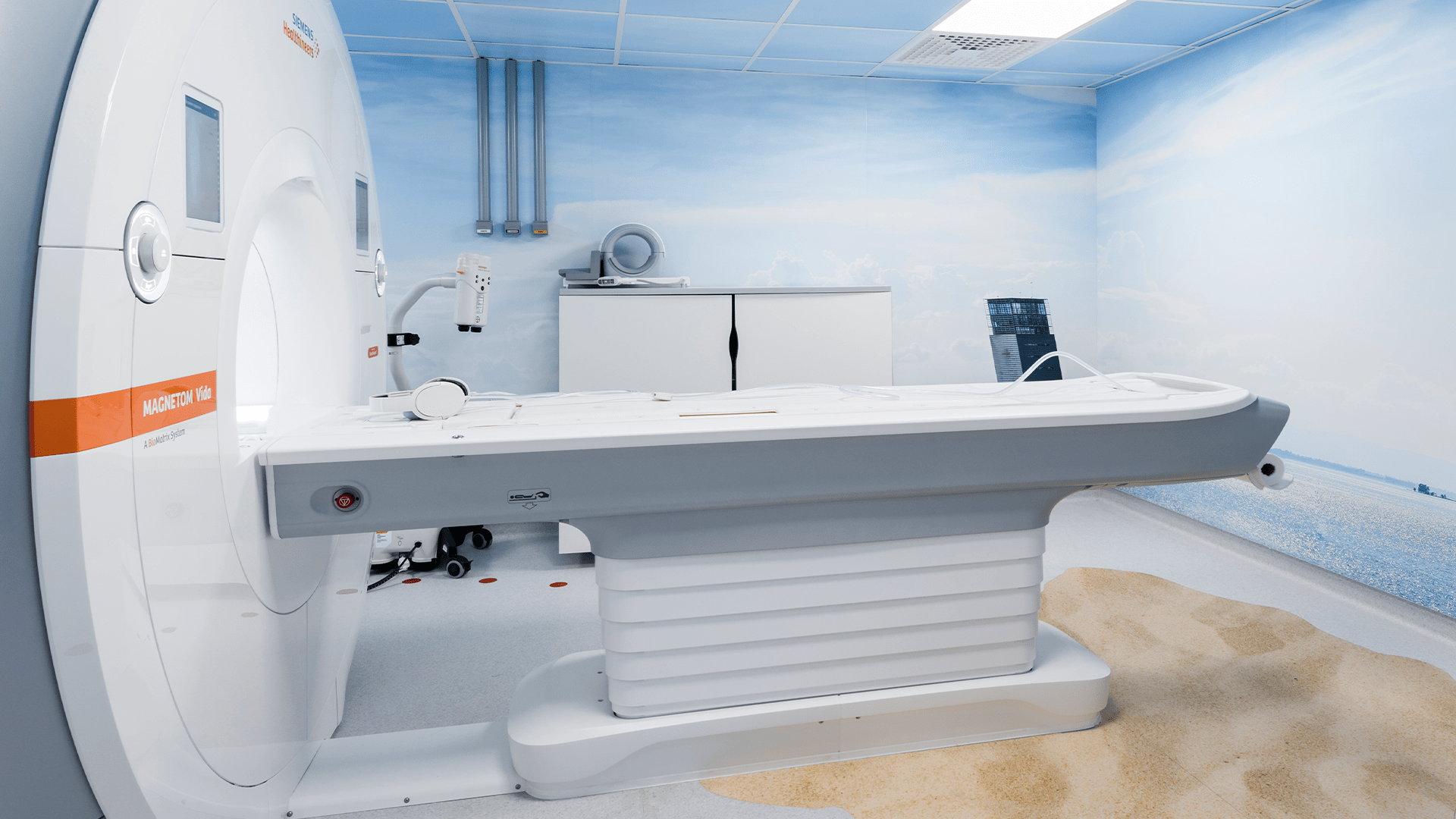
Migraines are diagnosed by a neurologist, by collecting the medical history and conducting physical and neurological exams. In some cases, the physician may use CT scanning or magnetic resonance imaging (MRI) to rule out other conditions. The diagnosis is confirmed when typical symptoms are present and test results do not indicate other underlying disorders.
In some cases, migraines are not the disease itself, but rather the symptom of a more serious condition. Neurological exams are always necessary when migraines present atypical manifestations, such as:
- Acute onset within seconds;
- Onset after the age of 50;
- Exponential increase in intensity and frequency;
- History of cancer;
- Weakened immune system;
- Fever or neck stiffness.
How are migraines treated?
Although there is no cure, migraines can be controlled effectively. When medical help is sought, the specialist often asks the patient to keep a migraine diary, describing the number and frequency of attacks, as well as possible factors that trigger them. This provides the physician with the necessary information to prescribe the most suitable and effective treatment.
Common medical recommendations may include:
- Medication therapy to relieve symptoms (such as painkillers, anti-inflammatories, antiemetics or triptans, gepants or monoclonal antibodies);
- Rest in a quiet and dark place;
- Applying pressure or cold on the pain site;
- Relaxation techniques, especially when stress is a trigger;
- Lifestyle changes, such as regulating sleep, exercising, giving up smoking, making dietary changes and reducing stress;
- Acupuncture;
- Homeopathy.
It’s important to remember that any treatment should always be prescribed by a physician, as the most suitable intervention depends on each individual case. What may have been effective for one person may not be for another.
Migraine: precautions
Taking certain precautions in everyday life can help minimise the impact of migraines, reduce the frequency of attacks and improve quality of life. We provide some recommendations below:
Maintain a regular sleep routine
Sleeping too little or too much can trigger migraine attacks. It’s important to keep regular bedtime and waking schedules to ensure sufficient and consistent rest.
Reduce stress
Stress is one of the principal factors associated with the onset of migraine attacks. Techniques like deep breathing, meditation, mindfulness or taking regular breaks throughout the day can help reduce accumulated stress.
Avoid intense sensory stimuli
Bright lights, loud noises and intense odours can aggravate or trigger migraines. Whenever possible, minimise the exposure to these stimuli, especially at times of heightened sensitivity.
Use medication properly
Medication should only be taken according to medical instructions. Excessive or improper use of painkillers can worsen attacks or lead to the development of medication overuse headaches.
Maintain regular medical follow-up
Follow-up in Neurology consultations enables the specialists to adjust treatment, monitor the condition and prevent complications, especially in cases of frequent or debilitating migraines.
How to prevent migraines
Although it’s not always possible to avoid attacks, some preventive measures can help better control migraines.
Identify triggers
Each person can present different triggers. Keeping a migraine diary helps identify patterns associated with attacks, such as foods, hormone changes, stress or sleep deprivation.
Avoid long fasting periods
Fasting for many hours can trigger attacks. The ideal is to maintain regular and balanced meals throughout the day in order to avoid attacks.
Maintain a balanced diet
In some people, certain foods can trigger migraines. Reducing alcohol and caffeine consumption and avoiding ultra-processed food can help prevent attacks.
Exercise regularly
Moderate and regular exercise helps reduce stress and improve general wellbeing, and can have a positive effect on migraine prevention.
Implement relaxation techniques
Activities like yoga, stretching, massages or breathing exercises help reduce physical and emotional tension, which are often associated with attacks.
Follow preventive therapy (when indicated)
In cases of frequent or extremely debilitating attacks, the physician may recommend preventive medication in order to reduce the frequency, intensity and duration of attacks.